Theseasonal downpours that soak the red dirt roads here nurtureclouds of mosquitoes that spread malaria. Researchers call it a forgotten epidemic: The parasitic disease kills more than 400,000 people each year. Most victims arechildren in Africa.
By Henry Wilkins
No hospital in this rural community has recorded a covid-19 death. But another menace fills graves on a grimly predictable schedule.
Theseasonal downpours that soak the red dirt roads here nurtureclouds of mosquitoes that spread malaria. Researchers call it a forgotten epidemic: The parasitic disease kills more than 400,000 people each year. Most victims arechildren in Africa.
The coronavirus pandemic, by contrast, has claimed about 130,000 lives on the continent in the past 15 months, according to World Health Organization estimates.
Yet only the coronavirus hascommanded a surge of global resources that fast-tracked vaccines, smashing development records and reshaping attitudes toward what is pharmaceutically possible.
Now scientists in Burkina Faso aim to harness that momentum to end what they see as the region’s more urgent threat.
“We are all frustrated in Africa to see how covid gets so much attention compared to malaria,” said epidemiologist Halidou Tinto, regional director of Burkina Faso’s Institute of Research in Health Sciences. “If malaria concerned the West, the attention would be much more focused.”
Tinto, 52, is leading clinical tests on the most promising injection against malaria yet — a shot found to be 77 percent effective for a group of Nanoro children over a 12-month trial, researchers reported this year in a study published in the Lancet.
The vaccine candidate, known as R21, is the first of its kind to cross the WHO’s 75 percent threshold, raising hopes and a pressing question: If Pfizer and Moderna can speed up dose deployment, why is this effort taking so long?
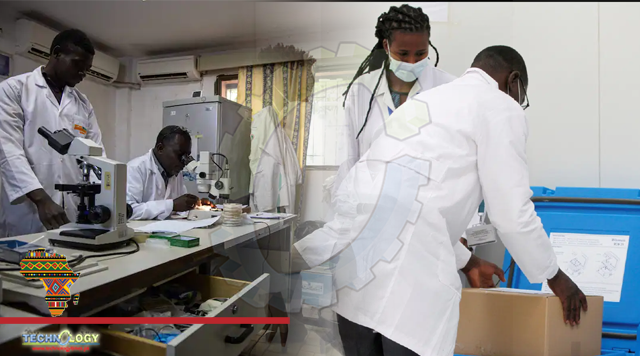
“Every second we delay the introduction of this vaccine, we lose more kids,” Tinto said at his office in Nanoro, where scientists nearby studied blood samples under microscopes, collecting the data required to move forward.
Work on R21, developed by Oxford University’s Jenner Institute, began in the United Kingdom more than a decade ago.
Now researchers are striving to secure prequalification from the WHO — a distinction that attracts funding and logistical support from global donors, and the first step for virtually every vaccine used in Africa. Regulatory approval from countries normally follows.
In the absence of a vaccine, other preventive measures have dominated the fight.
Malaria cases worldwide have fallen with the rise of rapid diagnosis, bed nets and better drugs: Global mortality dropped by 60 percent from 2000 to 2019, according to the WHO. Deaths in Africa decreased by nearly a half over that period. But progress since then has ground to a near halt.
Tinto and his colleagues say a vaccine is the missing piece.
Before the pandemic rush, the mumps inoculation held the record for fastest lab-to-authorization time: Four years, achieved in the late ’60s.
The coronavirus shots completed in months were aided by extensive research already conducted on similar viruses, as well as advances in manufacturing. But it was enormous sums of money that got them over the finish line.
The United States alone poured more than $9 billion into coronavirus vaccine development. The world spent $7.3 billion into malaria-related research and development from 2007 to 2018, according to the WHO.
Researchers blame the disparity on market forces: The countries most devastated by malaria tend to be the poorest.
“You’re not going to get malaria in England anymore, or the U.S., so richer countries, which have the research budgets to tackle these tropical diseases, have to spend the right amount of money to make an impact,” said Adrian Hill, director of the Jenner Institute. “It does seem odd that malaria, at least for Africa, is not considered an equivalent priority when there’s this huge number of children dying every year.”
The slowest stage of vaccine creation is what the Burkina Faso team is tackling now: efficacy and safety tests on people. Usually, that involves three phases, each larger and pricier than the last.
The pandemic doses took the same testing journey — just simultaneously. Pharmaceutical companies, flooded with cash, chose to absorb the financial risk of doing so.
Economic pain in wealthy nations spurred the burst of investment, said Julien Potet, a tropical disease policy adviser at Doctors Without Borders. The lesson: Spending blitzes can be astonishingly effective.
“It is crucial to increase funding for diseases like malaria that are far from being controlled,” Potet said. “Yes, there has been some progress. But threats like insecticide resistance, or resistance to medication, are looming.”
Malaria is a notoriously resilient killer. The parasite has been found in mosquitoes preserved in 30-million-year-old amber, meaning the disease has had ample time to mutate. Scientists have struggled for most of the past century to beat that genome puzzle.
Before R21’s favorable performance this spring, the previous best contender worked between a third and 66 percent of the time in a series of trials. The newcomer is built with more of the protein secreted by the malaria parasite when it enters the body.
By next year, the Jenner Institute should have enough safety data to apply for WHO prequalification, Hill said. Researchers in Burkina Faso and three other countries are now recruiting 4,800 participants for the next trial.
The Serum Institute of India, the world’s top producer of coronavirus vaccines, has already agreed to manufacture the malaria jabs.
WHO officials say they are open to it.
“It may well be possible to accelerate regulatory review,” said David Schellenberg, a science adviser for the WHO’s Global Malaria Program. “I think we’re all very keen to learn as many lessons from covid as possible.”
That norm-setting greenlight could take two years off the rollout, Tinto estimated. If malaria continues to kill at its current pace, he said, “that could save up to 800,000 lives.”
Emergency approvals, however, are up to the regulatory processes in individual countries.
Burkina Faso is one of six African nations that account for approximately half the world’s malaria deaths. The country of 20 million counts 11 million cases a year, which, on average, kill 4,000 people.
Cases spike with the wet season, when puddles turn to breeding grounds. Motorcyclists say the air is so thick with mosquitoes, it sometimes feels like they’re driving through rain.
The chief of Nanoro, Alassane Kondombo, said he has never known a time when malaria was not a huge burden for his community.
The coronavirus, by comparison, seemed like a mild nuisance. The local hospital has confirmed two cases, and neither were serious. Burkina Faso’sbiggest outbreak was in the capital, Ouagadougou, which recorded most of the nation’s 167 deaths.
“Malaria,” he said, “is by far the biggest concern for residents.”
Poverty is endemic in Burkina Faso, and five years of conflict, mostly in the countryside, has made it worse. Fighters linked to the Islamic State and al-Qaeda have forced more than a million people from their homes.
Many families cannot afford medication or gas money to get to a clinic. Infections deteriorate. Then comes tragedy.
On a recent afternoon in Ouagadougou, Karidjata Peszko, 19, a survivor of extremist violence, recalled her loss.
Three months ago, her 2-month-old daughter, Mariame, stopped breastfeeding. The young housewife took the baby to a clinic, where they spent four days. She couldn’t cover the medical bills. Mariame had severe malaria, and Peszko couldn’t cover the medical bills.
Her family lost almost everything when they fled their northern village to the capital.
“We stayed with her for six days while trying to find the money,” she said softly. “It was then she passed away.”
Originally published at The washington post